
Concentric And Eccentric Carved Costal Cartilage
A Comparison of Warping
David W. Kim, MD; Anil R. Shah, MD; Dean M. Toriumi, MD
Objective: To determine if a systematic, concentric graftcarving technique results in less warping than eccentric carving.
Methods: Costal cartilage from ribs 3 through 9 were harvested from fresh human cadavers. Concentric dorsal grafts were carved from cartilage obtained from one side of the cadaver (n=7) and eccentric grafts were carved from the opposite side (n=11). After carving, grafts were placed in saline sponges (isotonic sodium chloride) for 1 hour, and photographs were then taken from a lateral and a frontal view. Identical photographs were taken after 2 weeks of incubation in saline (36.7°C). The angle of curvature was measured from the photographs.
Results: More warping occurred in the eccentric group than the concentric group on lateral view at 1 hour (4.4° vs 0.4°; P_.001) and at 2 weeks (5.8° vs 1.4°; P=.003). Eccentric grafts progressively warped between the 1-hour and 2-week points.
Conclusion: Meticulous concentric carving of costal cartilage grafts may minimize the complication of graft warping. Arch Facial Plast Surg. 2006; 8:42-46
Author Affiliations: Division of Facial Plastic and Reconstructive Surgery, Department of Otolaryngology–Head and Neck Surgery, University of California, San Francisco (Dr Kim); and Division of Facial Plastic and Reconstructive Surgery, Department of Otolaryngology–Head and Neck Surgery; University of Illinois at Chicago (Drs Shah and Toriumi).
COSTAL CARTILAGE GRAFTing in rhinoplasty has gained increasing popularity in recent years. This technique is valuable when a significant degree of structural augmentation and support is needed in the nasal dorsum and tip. Saddle nose deformities, congenital nasal deformity, severe tip weakness or underprojection, rhinoplasty in nonwhite patients, and secondary rhinoplasty represent some of the scenarios in which this technique may be applied. Most commonly, the rib graft is used to create strong grafts to augment or support the nasal dorsum, tip, or septum. In addition, costal cartilage may be used in cases in which septal or auricular cartilage is not available for grafting.
Although alloplastic implants have been used to correct many of these deformities, increased risks of infection, extrusion, and foreign body reaction are associated with their use.1-3 Irradiated homograft costal cartilage is a good option for grafting, but studies have reported potential resorption over many years.4-6 Resorption would be a problem if the irradiated costal cartilage was used for structural grafting. An additional problem with irradiated rib is that it is difficult to obtain: there seems to be a shortage of this material in tissue banks. The use of nonirradiated autograft costal cartilage poses less risk of infection than use of alloplasts and less resorption than irradiated costal cartilage. The disadvantages of autograft rib cartilage include donor site morbidity, increased operative time, and a risk of graft warping. In reality, the risk of pneumothorax is extremely low if meticulous dissection is carried out to preserve the parietal pleura and underlying perichondrium. Therefore, the main risk of costal cartilage grafting is warping. This distortion of the graft may result in deformity of the nasal dorsum and/or tip and is one of the reasons many surgeons avoid using autograft rib cartilage.
Previous studies have examined the dynamics of cartilage warping. Gibson and Davis7 reviewed 46 medical charts of patients who had undergone costal cartilage augmentation of the nasal dorsum and determined that warping had not occurred. These authors carved concentric segments of cartilage to minimize the “interlocking stresses.” They were able to directly measure the degree of warping in costal cartilage and determine if there was a difference in the amount of warping dependent on the intervention to the costal cartilage. Fry8 demonstrated that protein polysaccharides within cartilage produce internal tensile stresses that cause the cartilage to change shape.
Harris and associates9 found that central portions of cartilage warped less than peripheral portions cut with a standardized block-cutting device. Costal cartilage was cut into 3.5_3.5_25-mm rectangular blocks. Adams et al10 also examined warping with an identical blockcutting device and similarly found that central portions warped less than peripheral portions, even in previously irradiated segments.
Previous studies have provided evidence that centrally carved grafts exhibit a decreased rate of warping compared with peripherally carved grafts. However, no study has described the application of this technique to grafts of the size, proportion, and dimension used in rhinoplasty. The present study tests the effect of concentric vs eccentric carving on the warping of grafts of the size and shape used as dorsal onlay grafts in rhinoplasty. It is our hypothesis that concentric carving of typical dorsal rhinoplasty grafts from costal cartilage will result in less graft warping than eccentric carving.
The timing of graft warping is another area of controversy. Reports conflict regarding when the actual warping occurs. Some studies suggest the distortion occurs in the first 30 minutes after carving, while others report that warping continues for weeks afterward.9, 10 The present study examines the timing of warping relative to the time of graft carving for the dorsal rib grafts.
Methods
62-year-old man. The entire cartilaginous portions of ribs 3 through 9 were removed from each side of the chest. For the oddnumbered ribs (Nos. 3, 5, 7, and 9), the left chest was used to obtain concentrically carved grafts and the right chest for eccentrically carved grafts. This was reversed for the even-numbered ribs (Nos. 4, 6, and 8). A total of 11 eccentric grafts and 7 concentric grafts were carved. This disparity in number occurred because only 1 concentric graft could be carved from each rib specimen, since the graft was obtained from the center of the segment, while 2 eccentric grafts could be obtained from some ribs5-7,11 because these were taken from the periphery of the segments. Though the final dimensions of a dorsal graft used in rhinoplasty vary depending on the clinical needs of the patient, a typical graft is overall canoe-shaped with a flat ventral surface and a gently curved dorsal surface. The lateral, cephalic, and caudal edges taper and the graft overall has proportions of roughly 8:2:1, length to width to height (Figure 1). The overall technique of concentric dorsal graft carving used in this study was the same as that used by the senior author (D.M.T.) in rhinoplasty.
A straight portion of the rib cartilage long enough to serve as a dorsal graft (3 to 5 cm) was identified and cut segmentally from the rest of the rib specimen. The perichondrial rind was then systematically shaved off with a scalpel. Because the axial orientations of the native rib segment and the final graft were not identical, graft carving could not be a truly concentric process. Instead, the cut end of the rib segment was inspected to determine the orientation in which the graft should be carved. The orientation that would allow for the most even carving to result in the final axial shape of the graft was chosen. That is, the rib segment was oriented in such a way that the amount of carved and discarded peripheral cartilage needed to create the graft is roughly equivalent at all points around the periphery of the final graft. For most rib specimens, the crosssectional shape was oval, making the orientation of graft carving a fairly intuitive process.

Figure 1.
The typical dorsal rib graft has
a tapered canoe shape and an 8:2:1
length to width to height ratio.
The eccentric grafts were carved from the periphery of each rib segment to a final size, shape, and orientation equivalent to the concentric grafts. A curved peripheral portion of the rib that matched the desired curved dorsal contour of the graft was identified.
Only the perichondrium was shaved from this dorsal curve. A straight cut was then made in the appropriate relationship to the dorsal curve to form the flap ventral surface of the graft. In some cases, the rib segment was wide enough to allow for 2 eccentric grafts to be harvested from the same specimen. For both concentric and eccentric grafts, the finalizing process of trimming, chamfering, and tapering the grafts into shape was completed with a 15 blade scalpel. This process created the characteristic smooth contour of the dorsal grafts used in rhinoplasty. At the completion of graft carving, all specimens were linear along the flat ventral surface when viewed laterally and along the central axis of the dorsal surface when viewed frontally. Each graft was overall a tapered canoe shaped with an 8:2:1 length to width to height ratio, representative of costal cartilage dorsal grafts used in rhinoplasty. After carving, all samples were wrapped in a roomtemperature saline-soaked sponge (isotonic sodium chloride) for 1 hour. After the saline bath, each specimen was removed and placed onto a blue background. Standardized digital photographs were taken from 20 inches away from a lateral perspective to assess for curvature of the ventral surface and 20 inches away from a frontal perspective to assess for curvature of the central axis of the graft. A measuring ruler was included in each photograph for reference. Each graft was then wrapped back into the saline sponge and placed into an incubator set at 98°F for 2 weeks. At 2 weeks, the grafts were photographed again in the same manner.
The photographs were then analyzed with a computer graphics program (Adobe Photoshop 7.0, San Jose, Calif). Initially, a line of curvature was identified and marked on the image. For the lateral views, the line of curvature was the actual ventral surface of the graft. For the frontal views, the line of curvature was plotted as a curve intersecting the midpoint of 7 lines of cross-section of the graft at the 1/8, 1/4, 3/8, 1/2, 5/8, 3/4, and 7/8 points along the length of the graft. For each line of curvature, a straight line was then plotted between the origin and termination of the curve. At the point of greatest divergence between the line of curvature and straight reference line, an intersecting perpendicular line was plotted and termed the line of divergence. The length of the straight reference line and the length of the line of divergence were then used to compute an angle of warping: angle of warping=inverse tangent of the length of the line of divergence/0.5_the length of the reference line (Figures 2, 3, and 4).
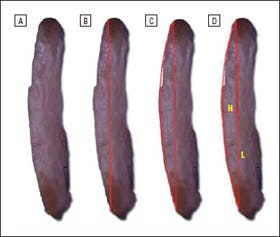
Figure 2.
Steps to assess degree of divergence from a straight reference line for the lateral view. A, Typical warped graft from the lateral view. B, Straight reference line is marked along the long axis of the graft. C, The curved surface of the graft is outlined intersecting the straight reference line. D, At the point of greatest divergence between the line of curvature and the straight reference line, an intersecting perpendicular line is plotted and termed the line of divergence or height (H). The length of the segment (L) represents the distance from the origin of the straight reference line and its intersection with H. The angle degree of divergence may be computed using the H and L values.

Figure 3.. Steps to assess degree of divergence from a straight reference line for the frontal view. A, Typical warped graft from the frontal view. B, The midpoint of 7 horizontal lines of cross-section of the graft at the 1/8, 1/4, 3/8, 1/2, 5/8, 3/4, and 7/8 points along the length of the graft are plotted. C, A line of curvature is placed intersecting these points. D, A straight reference line (in yellow) is placed from the origin and termination of the line of curvature. E, At the point of greatest divergence between the line of curvature and the straight reference line, an intersecting perpendicular line is plotted and termed the line of divergence or height (H). The length of the segment (L) represents the distance from the origin of the straight reference line and its intersection to H. The angle degree of divergence may be computed using the H and L values.
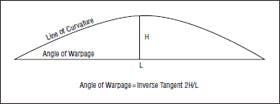
Figure 4. Method to assess angle of warping.
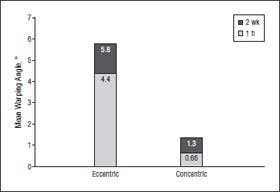
Figure 5. Mean angle of warping of grafts from the lateral view. Eccentric grafts demonstrated a greater angle of warping than concentric grafts at both time points. Values shown represent total angle of warping at each time point.
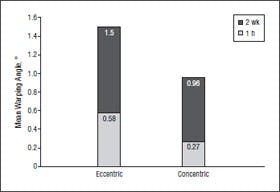
Figure 6. Mean angle of warping of grafts from frontal view. No statistical difference was found in the angle of warping between eccentric grafts and concentric grafts at either time point. Values shown represent total angle of
warping at each time point..
All data were then statistically analyzed using Microsoft Excel 2004. Comparisons of warping between concentric and eccentric samples at each time point were done with nonparametric Mann-Whitney tests. Nonparametric Wilcoxon signed- rank tests were then used to determine if significant differences in warping were present between the 1-hour and 2-week points for each group of specimens. All analysis was done separately for the frontal view and for the lateral view for each group of specimens at each time point.
Results
The mean±SD dimensions of the concentric rib grafts were as follows: length, 3.54±0.25 cm; width, 1.04±0.17 cm; and height, 0.47±0.08 cm. The mean±SD dimensions of the eccentric grafts were as follows: length, 3.45±0.29 cm; width, 1.01±0.17 cm; and height, 0.52±0.06 cm. There were no significant differences for any of the dimensions between the 2 groups. There was significantly more warping in the eccentric group than in the concentric group on lateral view both at 1 hour (4.4° vs 0.4°; P_.001) and at 2 weeks (5.8° vs 1.4°; P=.003) (Figure 5). There was no significant difference in warping between the eccentric and concentric grafts at either time point on the frontal view (Figure 6). Comparison of warping between the 1-hour and 2-week points for each group at each view was done to determine if warping continued beyond the immediate postcarving period. The results revealed that the eccentric grafts demonstrated a significant difference for both the frontal and lateral views between the 2 time points. The concentric grafts did not show significant differences between the 2 time points for either view (Table).
Comment
The problem of costal cartilage graft warping is well documented. Because these grafts often form the outward shape and contour of the nasal dorsum and tip, their deformation has serious consequences for the cosmetic outcome of rhinoplasty. Various measures have been taken to reduce the rate of rib graft warping. Irradiation of homograft cartilage has been reported to result in decreased rates of warping.4-6 However, given its potential for resorption, many surgeons are reluctant to use this material for structural grafting.4 This potential resorption is attributed in part to the lack of living chondrocytes in irradiated rib. Internal stabilization of rib grafts with Kirschner wires has been described by Gunter et al.13 In this report, the grafts stabilized with wires resulted in a significant reduction in graft warping in both cadavers and human patients. Three of 9 columellar struts initially placed, however, led to eventual wire extrusion. After modification of this technique, no further extrusions were reported.
Other studies describe the reduction of rib cartilage warping based on technique of carving and preparation. Gibson and Davis7 emphasized the importance of minimizing warping by balanced cross-sections of costal cartilage, which may be achieved by concentric carving. This concept was shown in their retrospective review of patient warping in 46 patients. Fry8 demonstrated that warping is in part caused by the internal tensile stresses produced by protein polysaccharides. Adams et al10 conducted a cadaver study in which uniform rectangular segments of cartilage were cut from either the periphery or center of rib cartilage specimens. Half of all specimens were subject to 1500 to 2500 rad (15-25 Gy) of irradiation prior to graft cutting. The results demonstrated a significantly higher degree of warping in the peripheral samples than in the central samples for both the irradiated and nonirradiated groups. No difference was found in degree of warping between the irradiated and nonirradiated groups. These grafts were thin rectangular segments
(25_3.5_3.5 mm) and did not resemble the dorsal grafts used in clinical rhinoplasty. In addition, they were cut using a standardized, experimental cutting device rather than carved in the manner that one would use in surgery. Although this study clearly demonstrated the principle that costal cartilage is less prone to later distortion when obtained from the center of the segment, it did not assess grafts of the size and proportions used in rhinoplasty.
Table. Comparison of Angles of Warping Between 1-Hour and 2-Week Measurements
| Graft Type | Mean Angle Difference, | ° P Value |
| Concentric | ||
| Frontal | 0.68 | 0.13 |
| Lateral | 0.95 | 0.06 |
| Eccentric | ||
| Frontal | 0.88 | 0.05 |
| Lateral | 1.35 | 0.05 |
The results of the present study demonstrate that significantly less warping occurs when dorsal grafts are carved using a concentric technique of cutting than with an eccentric technique. The difference of warping was significant on the lateral view (dorsal-ventral curvature). Although there was a greater mean angle of warping on the frontal view (side-to-side curvature) for the eccentric grafts than for the concentric grafts, this difference was not statistically significant. This discrepancy between the 2 views may be attributable to the relative thickness of the grafts in the different dimensions: the height (dorsal-ventral dimension) for each graft was about 0.5 cm, while the width (side-to-side dimension) was approximately 1.0 cm. The narrower dorsal-ventral thickness may make the graft more prone to warping in that direction. In clinical rhinoplasty, however, most dorsal rib graft warping is observed as a curvature of the dorsal line on the frontal view. This may be because the skin–soft tissue envelope over the nasal dorsum provides dorsal pressure onto the graft and likely compresses against forces of warping in the dorsal-ventral axis. Side-to-side warping may be less apt to occur than dorsal-ventral warping by virtue of innate graft dynamics, but it may be more clinically prevalent as there is less resistance against it provided by the soft tissue envelope. Though the present study did not specifically investigate the biomechanical mechanism of warping, we speculate that warping results from asymmetric forces of contracture exhibited by the fibrous architecture of the costal cartilage. Thus, cartilaginous specimens obtained from the center of a rib segment are less likely to bend preferentially toward one peripheral surface.
Another controversial issue is the timing of rib cartilage warping. Reports conflict regarding whether these grafts warp in the immediate postcarving period9,10 or if they continue to warp for weeks after carving.11 The present findings suggest that the eccentric grafts continued to warp both on the lateral view and frontal view after the 1-hour time point, as evidenced by further graft distortion at the 2-week point. The concentric grafts also demonstrated additional warping between the 1-hour and 2-week points for both views, but these differences were not significant. The timing of graft warping has implications on the management of the rhinoplasty patient who receives a rib graft. If most warping occurs immediately after carving, the surgeon may monitor the carved graft on the surgical back table prior to implantation. If no warping occurs after 30 to 60 minutes, one may be reasonably assured that no further warping will occur postoperatively. It is difficult to make such assumptions based on the present study or based on previous reports in the literature, given the inconsistent findings. In future studies, testing at more frequent time points and/or using timelapse photography over an extended period may better elucidate this issue.
The technique used by the senior author (D.M.T.) for carving costal cartilage involves a sequential carving process that takes over an hour. The carving is performed in stages throughout the operation. Initial carving is performed by removing most of the periphery of the harvested cartilage, and then the segment is allowed to soak in saline solution while other aspects of the operation are completed. Additional carving is then performed sequentially to shape the graft to its final form. As the graft is carved, any signs of warping are noted, and if a degree of curving is detected, additional carving is performed on the convex side of the curvature until the desired shape is achieved. The total process may take 2 or more hours before the graft is finally placed into the dorsal pocket just prior to closure.12 In summary, based on the results of this study, it is our conclusion that warping of costal cartilage grafts may be diminished through the systematic, concentric carving of cartilage from the center of rib segments. This principle may be applied to the carving of typical dorsal grafts used in dorsal augmentation rhinoplasty. Although the present study suggests that inherent forces of warping are more evident in the dorsal-ventral dimension of these grafts, we speculate that side-to-side warping is more clinically evident due to less soft tissue resistance in this dimension. It is unclear from this study or previous studies at what point after graft carving warping is most evident.
Accepted for Publication: July 27, 2005.
Correspondence: David W. Kim, MD, Division of Facial Plastic and Reconstructive Surgery, Department of Otolaryngology–Head and Neck Surgery, 2330 Post St, Fifth Floor, University of California San Francisco, San Francisco, CA 94115 ([email protected]).
Previous Presentation: This article was presented at the American Academy of Facial Plactic and Reconstructive Surgery fall meeting; September 19, 2003; Orlando Fla.
References
- Lovice DB, Mingrone MD, Toriumi DM. Grafts and implants in rhinoplasty and nasal reconstruction. Otolaryngol Clin North Am. 1999;32:113-141.
- Staffel G, ShockleyW.Nasal implants. Otolaryngol Clin NorthAm. 1995;28:295-308.
- Straith RE. Five long-term case reports (average 15 years) of saddle nose correction using cast Silastic implants. Plast Reconstr Surg. 1991;88:1064-1075.
- Welling DB, Maves MD, Schuller DE, et al. Irradiated homologous cartilage grafts: long-term results. Arch Otolaryngol Head Neck Surg. 1988;114:291-295.
- Schuller DE, Bardach J, Krause CJ. Irradiated homologous costal cartilage for facial contour restoration. Arch Otolaryngol. 1977;103:12-15.
- Dingman RO, Grabb WC. Costal cartilage homografts preserved by irradiation. Plast Reconstr Surg. 1961;28:562-567.
- Gibson T, Davis WB. The distortion of autologous cartilage grafts: its cause and prevention. Br J Plast Surg. 1951;10:257.
- Fry H. Nasal skeletal trauma and the interlocked stresses of the nasal septal cartilage. Br J Plast Surg. 1967;20:146-158.
- Harris S, Pan Y, Peterson R, et al. Cartilage warping: an experimental model. Plast Reconstr Surg. 1993;92:912-915.
- Adams WP, Rohrich RJ, Gunter JP, et al. The rate of warping in irradiated and nonirradiated homograft rib cartilage: a controlled comparison and clinical implications. Plast Reconstr Surg. 1999;103:265-270.
- Chafoo RAK, Goode RC. Irradiated homologous cartilage in augmentation rhinoplasty. In: Stuker FJ, ed. Plastic and Reconstructive Surgery of the Head and Neck, Proceedings of the 5th Internet Symposium. Philadelphia, Pa: Decker; 1989:297-300.
- Toriumi DM, Becker DG. Harvesting of autogenous tissue. In: Toriumi DM, ed. Rhinoplasty Dissection Manual. Philadelphia, Pa: Lippincott Williams & Wilkins; 1999:139-142.
- Gunter JP, Clark CP, Friedman RM. Internal stabilization of autogenous rib cartilage grafts in rhinoplasty: a barrier to cartilage warping. Plast Reconstr Surg. 1997;100:161-169.
Announcement
Clinical Trial Registration
In concert with the International Committee of Medical Journal Editors (ICMJE), Archives of Facial Plastic
Surgery will require, as a condition of consideration for publication, registration of clinical trials in a public trials registry (such as http://ClinicalTrials.gov or http:// controlled-trials.com). Trials must be registered at or before the onset of patient enrollment. This policy applies to any clinical trial starting enrollment after March 1, 2006. For trials that began enrollment before this date, registration will be required by June 1, 2006. The trial registration number should be supplied at the time of submission.
For details about this new policy see the editorials by DeAngelis et al in the September 8, 2004 (2004;292:1363-1364), and June 15, 2005 (2005;293:2927-2929), issues of JAMA.


